Article
 Andrew Webb, a professor of radiology and the director of the C.J. Gorter MRI Center at the Leiden University Medical Center in The Netherlands, visited the Beckman Institute this summer as part of a Beckman Institute Senior Fellowship.High-field and low, fast and slow, Andrew Webb has worked with MRIs of all shapes, sizes, and price points — each with a unique impact.
Andrew Webb, a professor of radiology and the director of the C.J. Gorter MRI Center at the Leiden University Medical Center in The Netherlands, visited the Beckman Institute this summer as part of a Beckman Institute Senior Fellowship.High-field and low, fast and slow, Andrew Webb has worked with MRIs of all shapes, sizes, and price points — each with a unique impact.
Webb is a professor of radiology and the director of the C.J. Gorter MRI Center at the Leiden University Medical Center in the Netherlands. He specializes in developing novel hardware for magnetic resonance imaging systems used for research and patient care.
This week, he wraps up a three-week-long fellowship at the Beckman Institute for Advanced Science and Technology. His visit was made possible through the Beckman Institute Senior Fellows Program, which offers established faculty members from other universities the opportunity to do short-term, interdisciplinary research onsite. This summer, Webb collaborated with researchers at the University of Illinois Urbana-Champaign and Carle Hospital to optimize the institutions’ shared 7 Tesla MRI scanner. He implemented best practices for imaging patients with implanted devices and developed new methods to improve image quality in specialized neuroimaging applications.
A veteran of Beckman and UIUC, Webb joined the Department of Electrical and Computer Engineering faculty in 1991 after earning his Ph.D. in medicinal chemistry at the University of Cambridge and completing his postdoc in radiology at the University of Florida. Webb became a full professor in 2001 and remained at UIUC until 2006. In 2019, he spent a sabbatical year at the Carle Research Institute for the formation of the Carle Illinois Advanced Carle Illinois Advanced Imaging Center Center and installation of the 7 Tesla MRI scanner.
The Beckman Institute’s ongoing Nadine Barrie Smith Memorial Fellowship honors Webb’s late spouse, herself a prominent researcher who earned her Ph.D. in biophysics from UIUC in 1996.
In this Q&A, Webb discusses his ties to the Beckman Institute, research on high-field MRI, and current efforts to increase access to MRI care.
Much of your research is focused on high-field MRI. What makes an MRI scanner high-field?
Standard clinical MRI systems operate at 1.5 and 3 Tesla, which, to put it in context, is 15-30,000 times stronger than Earth’s magnetic field. The stronger the magnet, the stronger the MR signal, and this allows us to generate images with finer resolution and often with better tissue contrast.
Essentially, high-field MRI generates the sharpest possible images.
Absolutely. And in certain clinical cases, that is critical. For example, if you’re looking for the first signs of a lesion or tumor, when the pathology is sub-millimeter in size. From the neuroscience perspective, within the cortex of the brain, you have lots of very fine, thin layers. With a standard scanner, the layers merge — but at a high field strength, you can see the activities in the individual layers, and their relationship. So, there are opportunities for basic science as well as clinical science.
For non-scientists, the jump from basic lab research to clinical care may be difficult to envision. Can you clarify that connection in the context of your work?
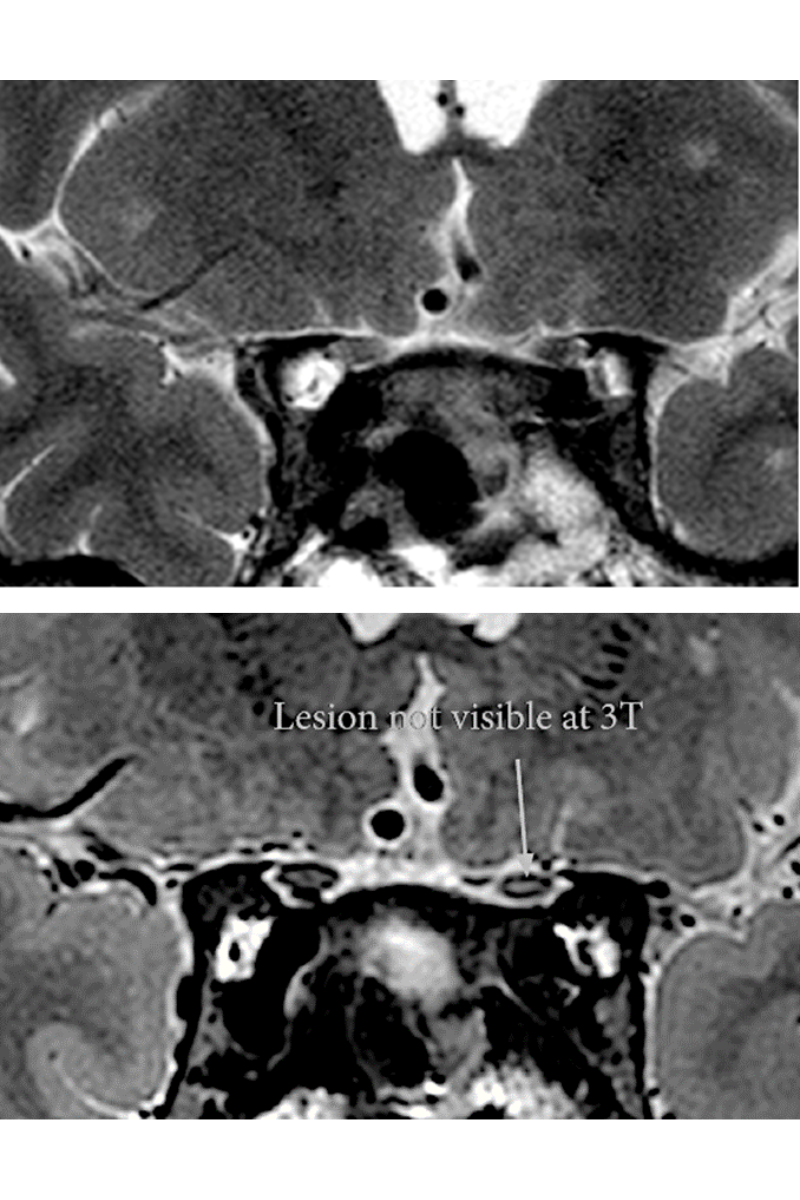 Two magnetic resonance images of the optic chiasm of a single patient, with the upper image generated at 3 Tesla resolution and the lower image generated at 7 Tesla resolution. The image taken at 7 Tesla resolution reveals a lesion not visible at 3 Tesla. Images provided by Andrew Webb.
Two magnetic resonance images of the optic chiasm of a single patient, with the upper image generated at 3 Tesla resolution and the lower image generated at 7 Tesla resolution. The image taken at 7 Tesla resolution reveals a lesion not visible at 3 Tesla. Images provided by Andrew Webb.One example which has had a direct link from lab to clinic is high-field MRI of eye tumors. There, it’s important to know the precise dimensions of the tumor and whether the tumor has broken through the back of the eye, which leads to metastasis. The hardware and data acquisition techniques necessary to produce detailed images of eye tumors didn’t exist, and so an undergraduate researcher in my lab developed a detector, based on a 3D-printed mask, that can wrap around a patient’s eye, and together with a faculty colleague in ophthalmology we developed techniques to overcome eye motion. This is an example of our engineering work in the lab having a very practical, diagnostic outcome — a patient could be treated differently because of our tools.
Did the chance to help patients inspire your research trajectory, or is it a happy byproduct of engineering?
It was both! This is one of the themes with MRI. It's a technical challenge, but in the end, you can get to the stage where you're doing something that makes a difference. It's nice when you see patients use what you build.
What technical challenges do you encounter in developing high-field MRI?
The human body is constantly moving. Cardiac scans are challenging because the heart is beating, and data must be acquired quickly, between beats, when it’s still. Eye movement poses a similar challenge. It’s also critical to ensure safe operation of such a powerful scanner. So, there’s a lot of engineering that needs to go into an MRI system, even when a commercial system is delivered. To get it to full capability, you need to design a lot of tools in-house, which requires a large team of dedicated faculty from many different departments.
And the opportunity to do team science is part of what brought you to Beckman.
It is indeed. There has always been a strong connection between Carle Foundation Hospital and Beckman. One of our focus areas this summer is implants. Whether you’re scanning healthy research volunteers or patients, many people have implants or metal dental retainers these days, and that is becoming more and more common. We want to learn more about how those implants and devices impact the scanning experience at 7 Tesla — both from the patient perspective and to produce the highest possible quality of images. So we are developing methods to test various circumstances and create best practices that are safe, reliable, and meaningful to research.
Where would you like to leave the Carle Illinois Advanced Imaging Center when you leave for the Netherlands? What is the best-case scenario?
A cutting-edge understanding of safety best practices and best practices for generating high-quality images. Ultimately, becoming more confident with different types of MRI scanning will increase the number of people who are able to undergo these scans, which will help to advance high-field MRI research, and expand the possibilities for the technology. We are also working with some new materials, termed metasurfaces or artificial dielectrics, which we believe can increase the image quality in brain scans acquired at 7 Tesla.
Even as your work expands the capabilities of high-field MRI technology, you’re also working to expand the availability of the physical MRI scanners themselves.
Yes. So, about 80 percent of my current work is trying to make MRI scanners sustainable and accessible in rural, under-resourced, or low-income communities and countries. That has been the biggest focus for my research group recently.
Where do we see a need for increased access to MRI?
Everywhere. Seventy percent of the world has zero access to MRI systems. And that really means no access — nothing at all. Even when it comes to conditions that are not difficult to diagnose, measuring the success of a particular treatment often ideally uses some form of non-invasive imaging.
What does sustainability look like in an MRI scanner?
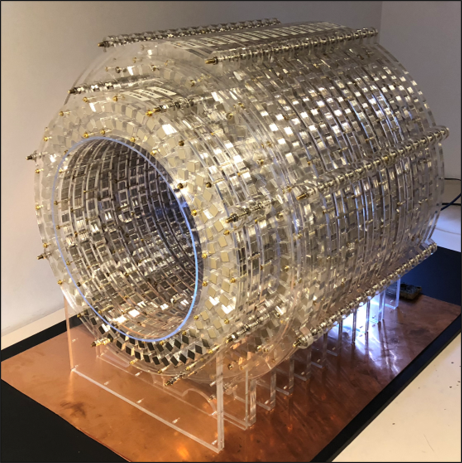 An example of a low-field MRI scanner developed by Andrew Webb and his colleagues. Image provided by Andrew Webb.
An example of a low-field MRI scanner developed by Andrew Webb and his colleagues. Image provided by Andrew Webb.It’s interesting because many things are more difficult to engineer in a simpler way. Thinking about cell phones, it’s quite easy to make a very good one. But how do you make one that does the basics well, and costs one percent of what it would normally — for an MRI scanner, that’s $10,000 instead of a $1 million — and is easy to use and repair? Because sustainability also means that an MRI system can be fixed without an exorbitant use of resources if it should break, which they often do.
Where do you see the future of this technology headed?
These MRIs are a lower field strength than the ones I am working with here at the University of Illinois, so the image quality will be a bit more blurred, a little bit grainier. However, these types of portable MRI systems can be extremely useful in places where there are simply no facilities currently available. The goal is to increase universal access to top-tier MRI scanners, and that these more portable, lower-field systems are ideal for triage and early diagnostics.
In some ways, your research is split between advanced techniques for higher-field MRIs and creative engineering for lower-field MRIs that are developing in a very different way. As a scientist, do you see a difference?
There is indeed a large difference in philosophy and applications that I am constantly aware of. But as a scientist, I see both projects as useful in their own ways and critical to addressing very, very different problems. The fact that the fundamental basis (i.e. magnetic resonance) is the same makes it interesting, and it means that we can make contributions to both the research and clinical areas.
Is there one aspect of your work that you find especially meaningful?
There’s a little bit of magic to the low-field side of it — of building every piece of an MRI system completely from scratch. In a way, we've sort of gone back to reevaluating the basics and saying: with all the improvements we've had in 30 years with electronics, and with image processing, how can we retain the transformative impact with a magnet that isn’t as strong? So, everything really goes in circles.
Do you see yourself circling back to the Beckman Institute?
Yes. If you look at everything I do and everything I’ve done, it’s always been with many kinds of people. So even though I’m in engineering, I came from a chemistry background, and at Beckman I ended up working with synthetic chemists, psychologists, civil engineers, veterinarians, cognitive neuroscientists, and many researchers from other disciplines. And why did I do that? Because they were here in Beckman. That idea of throwing everyone together is one reason why I really like the atmosphere.
There’s also the connection to Beckman that I have through my wife, who passed away some time ago, but we continue to see a lot of Beckman fellowships in her name. And that’s also why I keep coming back, to see the young people coming through. It’s the same thing with everyone here: there are always new styles, new research, new people, new ideas.
Beckman Institute for Advanced Science and Technology